The Long-Term Presence of Male Fetal Progenitor Cells: Implications for Health and Genetics
A recent study has unveiled a remarkable discovery regarding the presence of male fetal progenitor cells (mFPCs) in the bloodstream of mothers long after pregnancy. This research challenges traditional understanding and has significant implications for maternal health and genetics.
Researchers collected venous blood samples from 32 pregnant women and 8 nonpregnant women who had previously given birth to male infants, ranging from 6 months to 27 years postpartum. Using flow cytometry and PCR technology, they isolated and analyzed mononuclear cells for the presence of Y chromosome sequences, indicative of male fetal cells.
In pregnant women, male DNA was found in 13 out of 19 cases where they were carrying a male fetus. Strikingly, male DNA was also detected in 4 out of 13 pregnancies where the fetus was female, suggesting persistence of fetal cells from previous pregnancies.
Among nonpregnant women who had given birth to males, male DNA was detected in CD34+CD38+ cells in 6 out of 8 cases, including one woman whose last pregnancy dated back 27 years.
The study’s findings indicate that mFPCs can persist in maternal circulation for extended periods, potentially influencing maternal health and genetic dynamics. This phenomenon challenges conventional views on genetic inheritance and raises questions about its implications for future pregnancies.
Further research is needed to explore the health implications of these persistent fetal cells, as well as their impact on noninvasive prenatal testing (NIPT) accuracy. The study highlights the complexities of maternal-fetal interactions and underscores the need for continued investigation into the long-term effects of pregnancy on women’s health and genetics.
In recent years, scientific research has unveiled a fascinating and somewhat perplexing phenomenon: male fetal progenitor cells (mFPCs) can persist in a mother’s bloodstream long after pregnancy, sometimes for as many as 27 years postpartum. This discovery has significant implications not only for maternal health but also for broader aspects of human biology and genetics.
Understanding Male Fetal Progenitor Cells
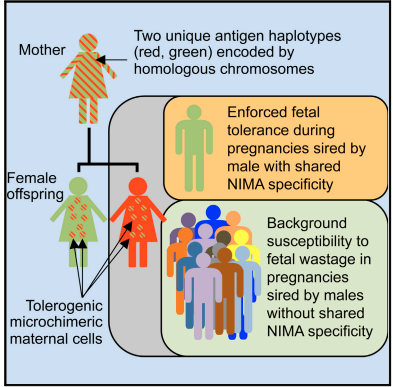
During pregnancy, a mother and her fetus exchange cells through a process known as microchimerism. This exchange allows fetal cells, including mFPCs, to enter the maternal bloodstream. These cells are thought to play a role in maternal immune tolerance toward the fetus, aiding in the successful progression of pregnancy. However, the persistence of these cells well beyond pregnancy has raised intriguing questions.
Research has shown that mFPCs can integrate into various tissues and organs of the mother’s body. They are particularly known to localize in the skin, liver, thyroid gland, and even the brain. This integration is a testament to the complex and dynamic nature of maternal-fetal interactions, extending far beyond the gestational period.
Long-Term Health Implications
While the presence of mFPCs in maternal tissues is a fascinating biological phenomenon, it also has potential implications for maternal health. Some studies have suggested that these cells may contribute to autoimmune diseases, such as rheumatoid arthritis and systemic sclerosis, by potentially triggering immune responses against the mother’s own tissues.
Moreover, the long-term presence of foreign cells in the maternal body raises questions about the effects on overall immune function. The immune system’s response to these cells over time could influence susceptibility to certain diseases and conditions, although the exact mechanisms are still under investigation.
Genetic Considerations and Social Implications
Beyond health concerns, the persistence of mFPCs also has intriguing genetic implications. It challenges the traditional understanding of genetic inheritance, as it suggests that a mother may carry genetic material from previous pregnancies long after they have ended. This could potentially influence future pregnancies and even impact the genetic diversity within a population.
From a social perspective, this phenomenon prompts us to reconsider the dynamics of reproductive relationships. It highlights that a mother’s body retains biological memories of past pregnancies, including those involving different fathers. While the direct impact on future children’s health is still a topic of research, it underscores the complexity of genetic relationships and the need for further exploration.
Ethical and Personal Considerations
In light of these findings, it becomes apparent why promiscuity or “sleeping around” may not be advisable from both health and genetic perspectives. Each sexual encounter, especially those resulting in pregnancy, leaves a lasting biological imprint on the mother’s body. The accumulation of mFPCs from different fathers over time could potentially complicate maternal health outcomes and blur genetic lines in unexpected ways.
Furthermore, the implications extend beyond individual health to societal norms and ethical considerations. Understanding the long-term consequences of microchimerism challenges us to rethink how we perceive reproductive choices and their impact on both maternal and offspring health.
Conclusion
The discovery of male fetal progenitor cells persisting in maternal blood for up to 27 years postpartum is a testament to the intricacies of human biology. It underscores the lasting impact of pregnancy on a mother’s body and raises important questions about health, genetics, and societal norms. While the full extent of these cells’ influence on health and genetics is still being explored, their presence serves as a poignant reminder of the profound connections forged during pregnancy and childbirth.
As we continue to unravel the mysteries of microchimerism, it is crucial to approach these discoveries with scientific rigor and ethical consideration. They provide a deeper understanding of human biology and challenge us to reconsider our perspectives on reproductive choices and their broader implications.